Hypertension‚ a global health issue‚ affects over 1 billion people worldwide‚ causing 7 million deaths annually. It is a multifactorial condition where elevated blood pressure leads to end-organ damage. Dr. Irvine Page’s Mosaic Theory explains hypertension as a result of interacting factors like genetics‚ lifestyle‚ and environment. Primary hypertension‚ the most common form‚ has no single cause‚ while secondary hypertension stems from identifiable conditions such as kidney disease or hormonal imbalances. Early diagnosis and management are critical to preventing complications.
1.1 Definition and Overview
Hypertension‚ or high blood pressure‚ is a common medical condition characterized by elevated blood pressure readings of 130/80 mmHg or higher. It is a major risk factor for cardiovascular diseases‚ stroke‚ and kidney damage. Hypertension can be categorized into primary (essential) and secondary forms. Primary hypertension‚ the most prevalent type‚ has no identifiable cause but is linked to factors like genetics‚ diet‚ and lifestyle. Secondary hypertension arises from underlying conditions such as kidney disease‚ hormonal imbalances‚ or certain medications. The Mosaic Theory‚ proposed by Dr. Irvine Page‚ suggests that hypertension results from the interaction of multiple factors‚ including renal mechanisms‚ vascular changes‚ and neurogenic influences. Early diagnosis and management are critical to preventing long-term complications and improving patient outcomes.
1.2 Classification of Hypertension
Hypertension is classified into two main types: primary (essential) and secondary. Primary hypertension accounts for 85-95% of cases and has no single identifiable cause‚ often linked to genetics‚ lifestyle‚ and environmental factors. Secondary hypertension‚ less common‚ stems from identifiable conditions such as kidney disease‚ adrenal gland disorders‚ or certain medications. Blood pressure readings are categorized as follows: normal (<120/80 mmHg)‚ elevated (120/80-129/80 mmHg)‚ stage 1 hypertension (130/80-139/89 mmHg)‚ and stage 2 hypertension (≥140/90 mmHg). Accurate classification is crucial for targeted treatment and improving patient outcomes. Understanding the type and severity guides clinical decisions‚ ensuring appropriate management strategies are implemented.
1.3 Historical Perspectives: The Mosaic Theory
The Mosaic Theory of Hypertension‚ introduced by Dr. Irvine Page in the 1940s‚ revolutionized understanding by emphasizing that hypertension results from multiple interacting factors. Page proposed that no single cause‚ but rather a combination of genetic‚ environmental‚ and physiological elements‚ contributes to elevated blood pressure. Over time‚ the theory has evolved‚ incorporating new insights into mechanisms like oxidative stress‚ inflammation‚ and the microbiome. This holistic view underscores the complexity of hypertension‚ guiding research and treatment approaches; The Mosaic Theory remains foundational‚ highlighting the need for comprehensive management strategies that address the interplay of various factors in individual patients.

Primary Hypertension
Primary hypertension‚ the most common form‚ accounts for 85-95% of cases‚ often linked to lifestyle‚ genetics‚ and environmental factors‚ with no single identifiable cause.
2.1 Characteristics and Pathogenesis
Primary hypertension is characterized by a gradual onset and asymptomatic nature in early stages. It involves complex interactions between genetic‚ environmental‚ and lifestyle factors. Key mechanisms include impaired sodium handling by the kidneys‚ leading to volume expansion and vasoconstriction. The renin-angiotensin-aldosterone system plays a central role in regulating blood pressure‚ with angiotensin II acting as a potent vasoconstrictor. Endothelial dysfunction and increased peripheral resistance are hallmark features‚ contributing to sustained elevated blood pressure. Genetic predisposition‚ dietary factors‚ and stress further exacerbate the condition. Over time‚ these factors lead to structural and functional changes in blood vessels and organs‚ perpetuating the hypertensive state.
2.2 The Role of the Renin-Angiotensin System
The renin-angiotensin system (RAS) is a critical regulator of blood pressure. Renin‚ released by the kidneys‚ triggers the conversion of angiotensinogen to angiotensin I‚ which is then converted to angiotensin II by angiotensin-converting enzyme (ACE). Angiotensin II is a potent vasoconstrictor and stimulates aldosterone release‚ promoting sodium retention and volume expansion. While circulating RAS is not the primary driver in essential hypertension‚ local tissue RAS in the kidneys‚ heart‚ and blood vessels plays a significant role. Activation of RAS leads to vasoconstriction‚ fibrosis‚ and inflammation‚ contributing to sustained hypertension. Therapeutic targeting of RAS with ACE inhibitors and angiotensin II receptor blockers (ARBs) effectively lowers blood pressure and reduces organ damage.

Secondary Hypertension
Secondary hypertension arises from identifiable causes‚ such as renal disease‚ endocrine disorders‚ or genetic mutations. It is less common but often treatable by addressing the underlying condition.
3.1 Identifiable Causes
Secondary hypertension is attributed to specific‚ often treatable conditions. Renal artery stenosis‚ a narrowing of arteries supplying the kidneys‚ disrupts blood flow‚ triggering high blood pressure. Endocrine disorders‚ such as hyperaldosteronism or Cushing’s syndrome‚ also contribute by altering hormone levels that regulate blood pressure. Additionally‚ pheochromocytomas‚ rare tumors of the adrenal gland‚ can cause episodic hypertension due to excessive catecholamine release. Other causes include thyroid dysfunction‚ sleep apnea‚ and certain medications. Identifying these underlying factors is crucial for targeted treatment‚ as addressing the root cause can often lead to significant blood pressure improvement or resolution.
3.2 Diagnostic Approach
The diagnosis of secondary hypertension involves a comprehensive evaluation to identify underlying causes. A detailed medical history and physical examination are essential to detect signs of endocrine or renal disorders. Routine laboratory tests‚ such as urinalysis and blood tests‚ help assess kidney function and hormone levels. Imaging studies‚ including renal ultrasound or angiography‚ may be used to identify structural abnormalities like renal artery stenosis. Additional tests‚ such as plasma renin activity or urinary metanephrines‚ are employed to diagnose specific conditions like hyperaldosteronism or pheochromocytoma. Early and accurate diagnosis is critical to guide targeted treatment and improve patient outcomes.

Pathophysiology of Hypertension
Hypertension involves complex interactions between kidneys‚ blood vessels‚ and the nervous system. Sodium retention‚ vascular resistance‚ and neurogenic mechanisms contribute to elevated blood pressure.
4.1 Kidney Mechanisms and Sodium Handling
The kidneys play a central role in regulating blood pressure through sodium and water balance. Impaired renal function or abnormal sodium handling can lead to hypertension. The renin-angiotensin-aldosterone system (RAAS) is activated in response to reduced renal blood flow or sodium depletion‚ increasing blood pressure by retaining sodium and water. Local renin-angiotensin systems in the kidneys further contribute to blood pressure regulation. Cross-transplantation studies show that kidneys from hypertensive animals can induce hypertension in normotensive recipients‚ suggesting a genetic link in sodium handling. Endothelial dysfunction and altered vascular responsiveness exacerbate these mechanisms‚ leading to sustained high blood pressure. These kidney-centric mechanisms highlight the critical role of renal pathophysiology in hypertension development and progression.
4.2 Vascular Changes and Endothelial Dysfunction
Vascular changes and endothelial dysfunction are key contributors to hypertension. The endothelium regulates blood vessel tone through nitric oxide (vasodilator) and endothelin (vasoconstrictor). In hypertension‚ reduced nitric oxide production and increased endothelin levels disrupt this balance‚ leading to vasoconstriction. Structural changes in arterioles‚ such as thickened walls due to smooth muscle cell contraction and remodeling‚ increase peripheral resistance. These changes are mediated by factors like angiotensin II and oxidative stress. Endothelial dysfunction also impairs blood flow regulation‚ contributing to sustained high blood pressure. Additionally‚ abnormalities in blood constituents‚ such as platelet activation and altered fibrinolysis‚ promote a prothrombotic state‚ further complicating hypertension. These vascular and endothelial alterations are central to the pathophysiology of hypertension‚ exacerbating its progression and complications.
4.3 Role of the Autonomic Nervous System
The autonomic nervous system (ANS) plays a significant role in blood pressure regulation. In hypertension‚ increased sympathetic nervous system activity leads to vasoconstriction‚ elevated heart rate‚ and increased cardiac output. The ANS mediates short-term blood pressure adjustments and responds to stress and physical activity. While the exact mechanisms driving sympathetic overactivity in hypertension remain unclear‚ factors such as lifestyle‚ genetics‚ and environmental influences are implicated. The interaction between the ANS and the renin-angiotensin system further amplifies blood pressure elevation. Therapeutic interventions targeting the ANS‚ such as beta-blockers and sympathetic inhibitors‚ highlight its critical role in hypertension management. Dysregulation of the ANS contributes to both the development and progression of hypertension‚ making it a key area of study in understanding the disease.
Risk Factors
Lifestyle factors‚ genetic predisposition‚ and metabolic syndrome significantly contribute to hypertension. Obesity‚ high sodium intake‚ and insulin resistance are key contributors‚ increasing cardiovascular risk globally.
5.1 Lifestyle Factors
Lifestyle factors significantly contribute to hypertension development. High dietary sodium intake leads to fluid retention and increased blood pressure. Obesity is a major risk factor‚ as excess body fat elevates blood pressure through insulin resistance and inflammation. Excessive alcohol consumption directly damages the autonomic nervous system‚ impairing blood pressure regulation. Physical inactivity contributes to weight gain and reduces the vasodilatory effects of exercise. Chronic stress triggers vasoconstriction and sodium retention‚ worsening hypertension. Poor dietary habits‚ such as low potassium and high saturated fat intake‚ further exacerbate blood pressure elevation. These modifiable factors are critical targets for prevention and management‚ highlighting the importance of lifestyle interventions in controlling hypertension.
5.2 Genetic Predisposition
Genetic factors significantly influence hypertension development‚ with family history increasing the risk. Specific genetic mutations can impair kidney function‚ sodium handling‚ or the renin-angiotensin system‚ key mechanisms in blood pressure regulation. Conditions like single-gene mutations in genes coding for aldosterone or sodium channels can cause inherited forms of hypertension. Additionally‚ genetic predisposition may enhance sensitivity to environmental factors‚ such as high salt intake or obesity. While most hypertension cases are polygenic‚ involving multiple genes‚ identifying these genetic markers aids in understanding disease mechanisms and tailoring therapies. Genetic predisposition underscores the complexity of hypertension‚ highlighting the interplay between inherited and lifestyle factors in its development and progression.
5.3 Metabolic Syndrome and Its Impact
Metabolic syndrome‚ characterized by obesity‚ insulin resistance‚ dyslipidemia‚ and glucose intolerance‚ significantly contributes to hypertension development. Central obesity leads to insulin resistance‚ promoting sodium retention and increased blood volume. Dyslipidemia and inflammation exacerbate endothelial dysfunction‚ reducing nitric oxide production and impairing vasodilation. Insulin resistance directly increases sympathetic nervous system activity‚ raising blood pressure. The clustering of these factors creates a pro-inflammatory and pro-thrombotic state‚ worsening vascular stiffness and peripheral resistance. Managing metabolic syndrome through lifestyle changes and pharmacotherapy is crucial to mitigate its impact on blood pressure and reduce cardiovascular risk. This interplay highlights the importance of addressing metabolic factors in hypertension management.

Organ Damage and Complications
Uncontrolled hypertension causes progressive damage to heart‚ brain‚ kidneys‚ and blood vessels‚ leading to severe complications such as heart failure‚ stroke‚ and chronic kidney disease.
6.1 Cardiac Involvement
Hypertension directly impacts the heart‚ leading to conditions like left ventricular hypertrophy (LVH) and heart failure. Increased afterload due to elevated blood pressure forces the heart to work harder‚ causing the myocardium to thicken. Over time‚ this can lead to diastolic dysfunction and eventually systolic failure. Neurohormonal activation‚ such as from the renin-angiotensin system‚ promotes fibrosis and further cardiac damage. Chronic pressure overload also increases the risk of coronary artery disease‚ exacerbating cardiac complications. Early intervention is crucial to prevent irreversible damage and improve outcomes in hypertensive patients.
6.2 Cerebral Complications
Hypertension significantly increases the risk of cerebrovascular events‚ including stroke and cognitive decline. Chronic high blood pressure damages cerebral blood vessels‚ leading to atherosclerosis and small vessel disease. This can result in ischemic or hemorrhagic strokes‚ with the latter often due to ruptured aneurysms. Additionally‚ hypertension is linked to white matter hyperintensities and silent brain infarcts‚ contributing to vascular dementia. The brain’s autoregulatory mechanisms may fail under prolonged pressure‚ causing hyperperfusion injuries. Early control of blood pressure is essential to mitigate these risks and preserve cognitive function.
6.3 Renal Implications
Hypertension significantly impacts renal function‚ leading to progressive kidney damage. Prolonged high blood pressure damages renal blood vessels‚ causing glomerulosclerosis and fibrosis. This impairs kidney function‚ reducing filtration capacity and leading to chronic kidney disease. The renin-angiotensin system plays a central role‚ as activation increases blood pressure and promotes fibrotic changes. Proteinuria‚ a hallmark of renal damage‚ often precedes overt kidney failure. Hypertensive nephrosclerosis accelerates disease progression‚ with fibrosis being a key pathological feature. Early intervention is critical to slow disease progression and preserve renal function. Antihypertensive therapies‚ particularly those targeting the renin-angiotensin system‚ are essential in managing renal complications.
6.4 Vascular Complications
Hypertension induces significant vascular changes‚ leading to endothelial dysfunction and arterial remodeling. Prolonged high blood pressure causes thickening of arterial walls‚ reducing vascular compliance and promoting atherosclerosis. This increases the risk of cardiovascular events‚ such as myocardial infarction and stroke. Endothelial dysfunction‚ characterized by reduced nitric oxide production and increased endothelin levels‚ further exacerbates vasoconstriction and inflammation. The renin-angiotensin system plays a key role by promoting vascular fibrosis and remodeling. Over time‚ these changes result in impaired blood flow and organ perfusion. Clinically‚ these complications manifest as increased arterial stiffness and heightened cardiovascular risk. Early intervention is crucial to mitigate vascular damage and reduce the likelihood of severe complications.

Diagnosis and Assessment
Accurate blood pressure measurement is crucial for diagnosing hypertension. A comprehensive clinical evaluation‚ including medical history and physical exam‚ identifies risk factors and target organ damage.

7.1 Clinical Evaluation
A thorough clinical evaluation is essential for diagnosing hypertension and assessing its impact. This includes measuring blood pressure accurately‚ reviewing medical history‚ and performing a physical exam. Lifestyle factors‚ such as diet and exercise‚ are evaluated‚ and symptoms of organ damage are assessed. The evaluation also considers the patient’s risk factors‚ like age‚ obesity‚ and family history. Additionally‚ the presence of comorbidities‚ such as diabetes or kidney disease‚ is noted. The goal is to identify underlying causes and determine the appropriate management strategy. Accurate assessment ensures timely intervention‚ improving outcomes and reducing complications.
7.2 Managing Hypertensive Crises
Hypertensive crises require immediate medical attention to prevent organ damage. These emergencies involve severely elevated blood pressure‚ often exceeding 180/120 mmHg. Acute management focuses on rapidly lowering blood pressure using intravenous antihypertensive drugs‚ such as sodium nitroprusside or clevidipine‚ under close monitoring. The choice of medication depends on the patient’s clinical condition and comorbidities. Continuous blood pressure monitoring in an intensive care setting is crucial to avoid excessive drops that could lead to ischemia. Additionally‚ identifying and treating underlying causes‚ such as pheochromocytoma or renal issues‚ is essential. Immediate intervention aims to stabilize the patient and prevent complications like stroke or cardiac failure. Prompt action is vital to improve outcomes and reduce mortality.
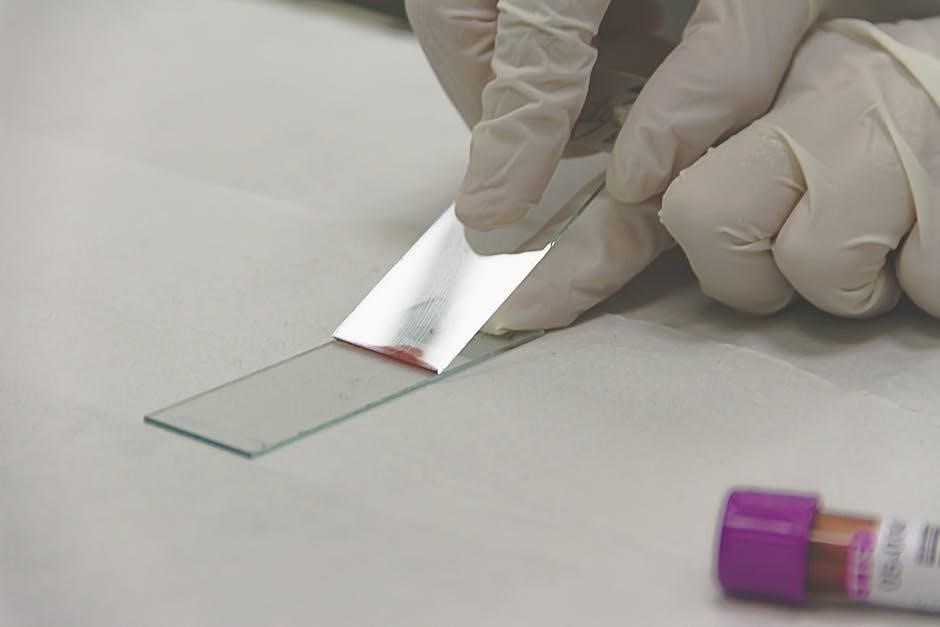
7.3 Role of Laboratory Tests
Laboratory tests are essential for diagnosing and managing hypertension‚ helping identify underlying causes and assess organ damage. Common tests include urinalysis to detect proteinuria‚ a marker of kidney involvement‚ and a complete blood count to rule out anemia or inflammation. Basic metabolic panels evaluate electrolytes‚ renal function‚ and glucose levels‚ while lipid profiles assess cardiovascular risk. Thyroid function tests and aldosterone-to-renin ratios may uncover hormonal imbalances contributing to hypertension. These investigations guide treatment decisions and monitor complications. Regular lab monitoring also helps track the effectiveness of therapy and detect potential side effects of antihypertensive medications. Accurate interpretation of these tests is critical for tailored management and improving patient outcomes.

Treatment Options
Hypertension treatment combines lifestyle modifications and pharmacological interventions. Lifestyle changes include dietary adjustments‚ increased physical activity‚ and weight management. Pharmacological options encompass various antihypertensive drugs tailored to individual needs. Regular monitoring ensures optimal blood pressure control and minimizes complications.
8.1 Lifestyle Modifications
Lifestyle modifications are the cornerstone of hypertension management‚ emphasizing sustainable changes to reduce blood pressure and improve overall health. Key interventions include adopting a balanced diet low in sodium and high in fruits‚ vegetables‚ and whole grains‚ such as the DASH diet. Regular physical activity‚ like moderate-intensity exercise for at least 30 minutes most days‚ is crucial. Weight management through calorie reduction and increased mobility helps lower blood pressure. Limiting alcohol intake and avoiding smoking are also essential. Stress management techniques‚ such as yoga or meditation‚ can further support blood pressure control. These modifications not only address hypertension but also reduce the risk of cardiovascular diseases‚ often delaying or reducing the need for pharmacological treatment.
8.2 Pharmacological Interventions
Pharmacological interventions are tailored to individual patient profiles and hypertension severity. First-line treatments often include renin-angiotensin system inhibitors‚ such as ACE inhibitors or angiotensin II receptor blockers (ARBs)‚ which reduce blood pressure by relaxing blood vessels. Calcium channel blockers (CCBs) are another primary option‚ particularly effective in older adults and those with certain comorbidities. Thiazide diuretics are commonly used‚ especially in volume-dependent hypertension. Beta-blockers may be prescribed for patients with heart conditions like arrhythmias or post-myocardial infarction. Aldosterone antagonists are considered for resistant cases. Combination therapies are often necessary to achieve target blood pressure levels‚ enhancing efficacy and minimizing side effects. Personalized treatment plans ensure optimal outcomes and adherence‚ addressing underlying conditions and lifestyle factors.

Special Populations
Hypertension management varies in special populations‚ including those with resistant hypertension‚ children‚ and pregnant individuals‚ requiring tailored approaches to address unique physiological and clinical challenges effectively.
9.1 Resistant Hypertension
Resistant hypertension refers to high blood pressure that remains uncontrolled despite the use of three or more antihypertensive medications‚ including a diuretic‚ at optimal doses. It is a challenging condition that affects a significant portion of hypertensive patients. The underlying causes can be primary or secondary‚ with contributors such as kidney disease‚ hormonal imbalances‚ or obstructive sleep apnea. Diagnosis involves confirming adherence to medication and identifying any secondary causes. Lifestyle modifications‚ such as dietary changes and increased physical activity‚ are often recommended. Treatment may include additional medications or procedures like renal denervation. Regular monitoring is essential to prevent complications and improve outcomes in this high-risk population. Managing resistant hypertension requires a tailored and multidisciplinary approach.
9.2 Hypertension in Children
Hypertension in children is a growing concern‚ often secondary to underlying conditions like kidney disease‚ hormonal disorders‚ or genetic factors. Primary hypertension is less common in children but can be linked to obesity and lifestyle factors. Early diagnosis is critical‚ as untreated hypertension can lead to long-term cardiovascular and renal complications. Blood pressure measurements must be interpreted using pediatric-specific percentiles. Ambulatory blood pressure monitoring is recommended for accurate diagnosis. Lifestyle modifications‚ such as dietary changes and increased physical activity‚ are the first-line treatment. When medications are required‚ careful selection is needed to minimize side effects. Managing hypertension in children requires a comprehensive approach to prevent complications and ensure healthy growth and development. Regular follow-ups are essential to monitor progress and adjust treatment plans as needed.
9.3 Hypertension During Pregnancy
Hypertension during pregnancy is a significant condition that can lead to complications for both mother and fetus. It is classified into gestational hypertension and preeclampsia‚ with the latter being more severe. Risk factors include a history of hypertension‚ obesity‚ and multiple pregnancies. Regular prenatal check-ups are crucial for early detection. Untreated hypertension can result in premature birth‚ low birth weight‚ and maternal organ damage. Management strategies include lifestyle modifications and‚ in severe cases‚ medication. Close monitoring of blood pressure and proteinuria levels is essential to prevent progression to preeclampsia. Timely delivery is often necessary in severe cases to ensure the safety of both mother and baby. Hypertension in pregnancy requires a multidisciplinary approach to minimize risks and improve outcomes.
